Research Areas
Magnesium and Head Injury
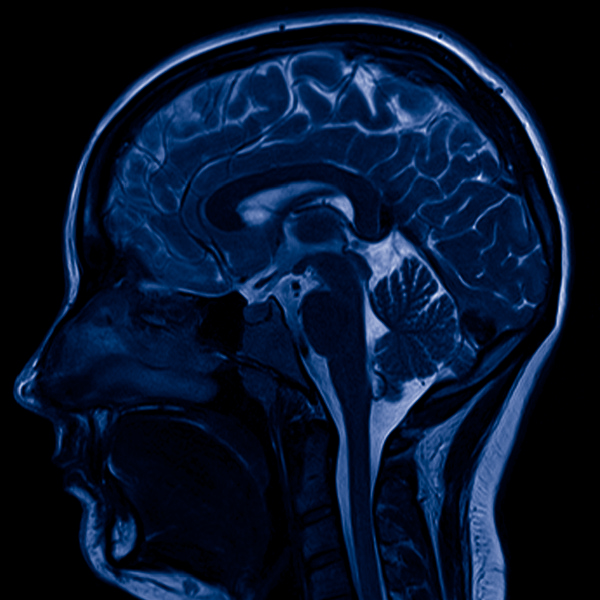
Purpose of Study: Does Early Intravenous Magnesium Sulfate Administration Improve Neurological Outcome In Patients Sustaining Acute Moderate And Severe Closed Head Injury
Background: Administration of intravenous magnesium salts have been shown to improve neurologic outcome after traumatic brain injury (TBI). Previous studies were done using experimental TBI in rats and it was shown that magnesium can attenuate the secondary injury cascade that occurs after TBI leading to impaired cellular metabolism. Free intracellular magnesium after TBI falls hours after injury and continues for several days. To date there has not been a prospective study using magnesium in the early post injury period and correlating its effect on neurologic outcome. The aim of this study is to show that the use of intravenous magnesium sulfate within four hours after TBI and its continued daily use for 5 days will result in better neurologic outcomes in human subjects sustaining accidental severe and moderate TBI.
Traumatic Brain Injury in the Inland Empire
Abstract: Approximately 50,000 residents die each year as a result of traumatic brain injury (TBI) in the U.S. Many survivors of TBI are left with debilitating brain damage resulting not only in severe physical and cognitive disabilities, but also with major social and financial problems. Since 1979, a decline has continued in TBI-related deaths and during 1989-1998, TBI-related deaths declined 11.4%, from 21.9 to 19.4/100,000. Our study reports the epidemiology, trends, and financial implications in TBI-related mortality and morbidity during 2001-2004 in San Bernardino and Riverside counties and compares them with national trends.
Introduction and Background Information:
In June 1979, a pilot phase study named The National Traumatic Coma Data Bank was started in efforts to collect data on severe non-penetrating traumatic head injury in order to address critical questions relating to the functional outcome of these patients. In response to the information generated by this pilot study, the Traumatic Brain Act of 1996 (Public Law 104-166) was passed and authorizes State surveillance systems to obtain information on the number of people affected by Traumatic Brain Injury (TBI), the causes of these injuries, and their severity. The following information has been obtained from this act:
- 230,00 people are hospitalized and survive
- 50,000 people die
- 80,000 to 90,000 people experience long-term disability
As the cumulative result of past TBIs, an estimated 5.3 million men, women, and children are living with a permanent TBI-related disability in the U.S. today. TBI is a major cause of morbidity and mortality in the U.S and mostly results from1, 2:
- motor vehicle accidents
- falls
- assaults
- sports injuries
Between 1989-1998, 53,288 annual deaths among U.S. residents were associated with TBI for a rate of 20.6/100,000 population3. These injuries have both short-term and long-term effects on individuals, their families, and society and their financial cost is enormous. According to one study, the annual economic burden in the U.S. was estimated at $56 billion in 2001.4
With approximately 5.3 million Americans who live with a TBI-related disability, the financial cost is only part of the burden. The long-term impairments and disabilities associated with TBI are grave and the full human cost is incalculable. Yet because these disabilities are not readily apparent to the public - unlike a broken arm, for example - TBI is referred to as the invisible epidemic. Individuals may suffer lifelong disabilities of physical, cognitive, and psychosocial functioning, often permanently altering a person's vocational aspirations and having profound effects on social and family relationships.
During 1989-1998, TBI-related death rates had declined in all age groups except persons ³75 years old who experienced increased death rates and had the highest death rate of any age group. The highest incidence of TBI is among persons 15 to 24 years of age and people 75 years and older, with males experiencing 3 times higher TBI-related death rates as compared to females. Declines of 13% in males and 7% in females were seen during 1989-1998 period. TBI-related death rates were highest among American Indian/Alaska Natives at 27.2 deaths/100,000 population, however, this group experienced a 13% decrease during the period. Blacks experienced the 2nd highest TBI-related death rate at 25.0 deaths/100,00 population and whites averaged 20.1/100,000 population. The greatest decrease in TBI-related mortality occurred in blacks (20%), with whites experiencing a 10% decrease.
The three leading external causes of TBI-related deaths were motor-vehicle-related, fall-related, and firearm-related, accounting for 40%, 34%, and 10% respectively. The leading causes of TBI-related death differed among specific age groups: fatal motor-vehicle injuries were the leading cause of TBI-related deaths among children and youths aged 0-19 years (62%), fatal firearm-related injuries were the leading cause among adults aged 20-74 (52%), and fatal fall injuries were the leading cause among adults ³75 years (46%).
Our analysis will examine and compare the more recent trends in Riverside and San Bernardino county (RSBC) TBI mortality to available CDC data, more specifically, 1) trends of RSBC TBI-related deaths during 2001-2003 as a percent of specific ICD-9 injuries, as a percent of all deaths and as a percent of trauma deaths, 2) describe differences in RSBC risk for death by age, sex, and race, 3) describe RSBC trends among the leading causes of TBI-related death: firearm-related injuries, motor-vehicle-related injuries, and fall-related injuries, 4) describe RSBC trends in location of the occurrence of injury and, 5) approximate the financial expense of RSBC medical and government assistance.